This question usually pops up in every mind while talking about any digital health intervention. This thought makes everyone think several times before implementing any new digital initiative. “Adoption” is a major challenge that everyone should take up in the limelight for the current digital revolutionary journey coming ahead.
Discussing India’s healthcare access and quality index according to the Lancet journal it holds its position at 145 out of 195 countries. Front line healthcare workers are the first line of contact in India’s healthcare system. The Active social health activists (ASHAs), Auxiliary nurse midwives (ANMs) and Anganwadi workers (AWWs) usually fall under the cadre of frontline health care workers in India. Most of the FHWs in India are using m-health interventions as one of the tools in providing quality access to healthcare services in India. On the other hand, most of the m-health platforms are aligned towards mother and child health. There are several m-health platforms in India that are being used at frontline level. Not only this they are embedded with various tools and clinical decision support systems that help in tracking high-risk pregnancies, record management, antenatal care visits, scheduling, generating referrals, training, monitoring and end-to-end patient management.
In India the major challenge in providing health care service is mostly confined to the rural areas and maternal and child health is one of those concerns that needs to be tackled. Various states has leveraged these m-health platforms in the tracking of mother and child health-related issues and providing training as well as front line level. But the biggest dilemma is are they being implemented well? Are they helping out in bringing the potential of these m-health interventions? Answering these questions will always remain as difficult till we come out with the solutions to overcome the major deterrent that is “Adoption”.
Talking About Challenges
If we articulate about some of the challenges in adoption it can be broadly portrayed in terms of:
- Technical issues
- Healthcare worker readiness
- Healthcare system readiness
Technical issues: Technical issues are one of the major deterrents that can lead to the failure in the whole system further leading to less or no adoption towards these online platforms. Complex designing of these health platforms that may influence them to take a back step towards the usage. Other issues may depend upon the features, how it is operated and up to what extent it is easier for them to update the fields in the system. There may be several other concerns like the phone getting heated up, or the phone freezing up, technical presentation (mobile friendly), touch screen etc.
Healthcare worker readiness: This may be understood well in terms of the perceived usefulness and perceived ease of use with some of the examples.
Perceived usefulness: They usually think that what is the purpose of updating the same field electronically while they are already doing by writing in the paper? Will it be beneficial for them in improving their service delivery if yes then how? And how much do they believe that using these systems would require less comfort and up to what extent?
Perceived ease of use: Due to the complex functionality of the device or system they may not appreciate using it. Is the device developed in alignment with their workflow? Or this may be the result of technical issues also they are facing while using it.
Apart from this lack of understanding, education, attitude towards the technology proficiency and self-efficacy in utilizing these tools. While working in rural and confined settings, they can suffer from low self-confidence and motivation and equally the perception of target communities towards them can also have an impact towards adoption.
Healthcare system readiness: This comes as an overall backend support for the FHWs in adopting these tools. Current health care policies and various health care institutions are not into the enforcement of these mhealth interventions. This may be due to the lack of standardised protocols for the usage of these tools. On the other hand, the poor network access in remote areas, poor access to electricity and lack of proper infrastructure or maintenance cost of the online platforms comes under the impoverished healthcare system. For example, the majority of FHWs also faced problems with the network, internet when it came towards synchronizing the data entered with the servers. Further, most did not have access to electricity sources in their centres to charge their phones. One of the studies stated that the AWWS usually work in AWCs and reported they don’t have ports or electricity sources from where they can charge their mobile phones.
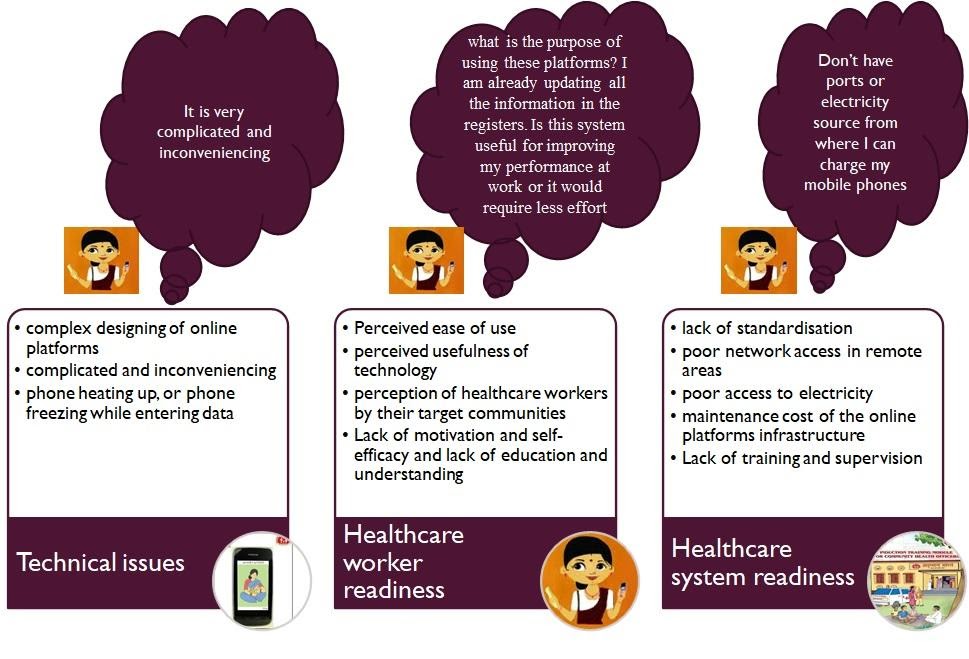
Challenges in adoption
Heading Towards Solution
Now the discussion lands up towards the solution on how we can make FHWs geared up with the revolutionary digital health practices. If we talk about the solutions we need to think accordingly and specifically at each level.
- Strategic level (at the time of planning)
- Operational level (requirements before the implementation)
- Frontline level (during implementation)
Strategic level: It is the first step that must be taken into consideration while implementing any of the interventions into the field. This usually includes planning and organizing of all the tasks and resources accordingly. Prerequisites during the planning must be clear in terms of value and workflow. Value usually encompasses the scope and how the usage of health intervention will benefit them. The aim of the overall process must be well communicated with the users as well. In terms of workflow the interventions that are being subjected to the users must align with what they usually undergo in providing services to the population. Healthcare policy acts as a lever in forming overall strategies. Therefore, standardised policy and regulations must be followed to maintain the main aspects of digital ecosystem i.e.; interoperability, data privacy and data management. Various other factors must also be considered like demographic, social, economic, etc. while formulating out the strategies.
Operational level: Before the intervention gets implemented at the ground level some of the key operational factors must be taken into the concern. For example, while implementing the mHealth intervention in any low-resource setting one must have adequate resources at the backend. Proper infrastructure, adequate supply of electricity, internet coverage with sufficient speedy networks and resources for providing training and technical support. We should also look into the fact that the tool they will be using should be user friendly and with not very complex functionality.
Frontline level: It becomes a very compelling factor in terms of adoption. One is directly in-contact with the healthcare workers. Continuous hand holding, motivating them through behaviour change communication (BCC), developing trust around the users act as the most important action point in addition in creating a sustained digital initiative on a large scale. Like the top leaders can be identified among them in terms of the beneficiaries they have updated so as to keep constantly engaged and motivated. Monitoring and evaluating their work outputs in terms of creating a daily scoreboard. Making them realize the scope, should be made clear to the Healthcare workers. When the users witness that online intervention can be taken as an encouraging means to accelerate the administrative processes, it is usually welcomed by them and easily adopted.
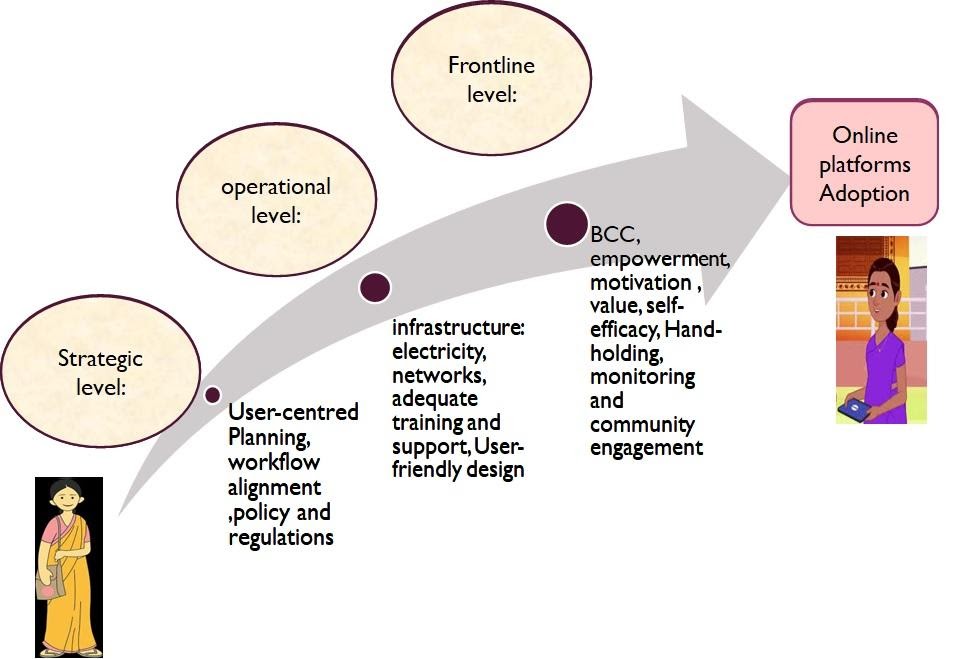
Solution towards adoption
Delivery of services to citizens through “online mode” is at the core of the overall electronic health ecosystem being talked about. Major I.T. Initiatives by the Ministry include various health initiatives for improving efficiency and efficacy of public health care across the country under the Digital India Program. For example- Govt of India has initiated “The Integrated Government Online Training (I GOT) -Diksha platform is being used to conduct seamless training sessions for healthcare professionals across the country. ECHO India has partnered with premier government healthcare institutions in its efforts to strengthen the emergency response to COVID-19 with consistent capacity building programs for healthcare professionals, including doctors, nurses, ASHA workers and paramedics by conducting virtual training sessions with their partners. Thus, there are still limitations, despite the existence of theories on technology usage in the workplace, the evidence regarding these interventions in terms of how they usually affect performance of FWHs and the evaluation of efficiency of services delivered through this is still missing.
Tamanna Sachdeva is presently associated with Tech Care for All as Business Analyst Healthcare. Her areas of interest are mainly in healthcare research and program management.

How amazingly written. Fantastic work. Thanks for sharing this knowledge.