The detrimental effect of the outbreak of COVID-19[the disease caused by Severe Acute Respiratory Syndrome coronavirus 2 (SARS-COV-2)] was evident not only on global healthcare systems but also on other aspects of human life.
The World Health Organisation (WHO) declared the COVID-19 outbreak as a global emergency on 30th January 2020. According to various scientific literatures, and a response to ‘flatten the curve’ governments have enforced border shutdowns, travel restrictions and quarantine in countries which constitute the world’s largest economies.All these factors have anticipated the fears of an impending economic crisis and recession.
The COVID-19 pandemic has caused an unprecedented challenge for healthcare systems worldwide with healthcare workers as the frontline warriors .
In upcoming times there may be a higher surge in cases reporting critical situations or may be even fatalities due to previously existing illnesses like Chronic Heart Failure, Chronic Renal Failure, COPD, etc. getting complicated because of improper or not adequately managed.
Several reports have shown the predicamemt of patients having chronic diseases and those require proper medical maneuvering other than COVID-19 infected patients.The overall revenue generation for hospitals and healthcare sectors were greatly affected e.g an official data from a 350 bedded hospital in NCR reports more than 50 % reduction in bed occupancy rate and more than 60 % reduction in routine elective procedures thus making the system very fragile.
Maharashtra Govt. has undertaken 80 percent of private hospital beds with capping of treatment costs Another such step has been taken by the Delhi Govt which has directed the private hospitals with capacity of 50 beds or more to provide 20 % of its total capacity for COVID-19 patients.
With the prevalence of such regulations, adequate measures are taken to safeguard the workforce of the organization. With such regulations, it becomes foremost important to take adequate measures to protect our workforce amid this health crisis as they are the only weapons all through this fight. For enabling life towards getting near to normal , first thing that has to be made sustainable is the healthcare system.
THE PROBLEM STATEMENT
- Patients with similar symptoms (influenza like symptoms) with pre-existing conditions like cardiac ailments and respiratory issues, are facing lot of trouble in getting routine management as well as emergency management because of projected COVID 19 stigma
- Upcoming conditions with similar presentation like Dengue, Malaria in South East Asian countries will make situation more complicated thus pose further challenges in healthcare system
- Healthcare workers (HCWs) has to embrace the the Quarantine in masses because of accidental exposure from a patient tested positive after routine admission
- Collapse of health system in terms of providing adequate health services and revenue to sustain hospitals viability
In short our health system includes both public sector and corporate sector are facing issue at every step whether it is:
- Containment of disease
- Proper handling to emergencies due to non COVID-19 chronic illnesses
- Protection of HCWS (almost 321 HCWs has been tested positive across DELHI)
- Sustainability
OBJECTIVES
- Combat ongoing crisis in best possible and efficient mannerto minimise the incidence of COVID-19 infection among HCWs
- Proper redressal of Patients suffering from chronic illnesses and impending life threatening emergencies related to such illnesses
- Anticipate upcoming seasonal illness like Dengue and Malaria and take optimum measures to reduce chances of further crisis with these upcoming health threats
- Develop a sustainable system where both the public health sector and private sector collaborate to fight this Pandemic crisis
- Develop a system where the corporate health system reaches their maximum capacity in terms of services and also the revenue
POLICY SUGGESTIONS
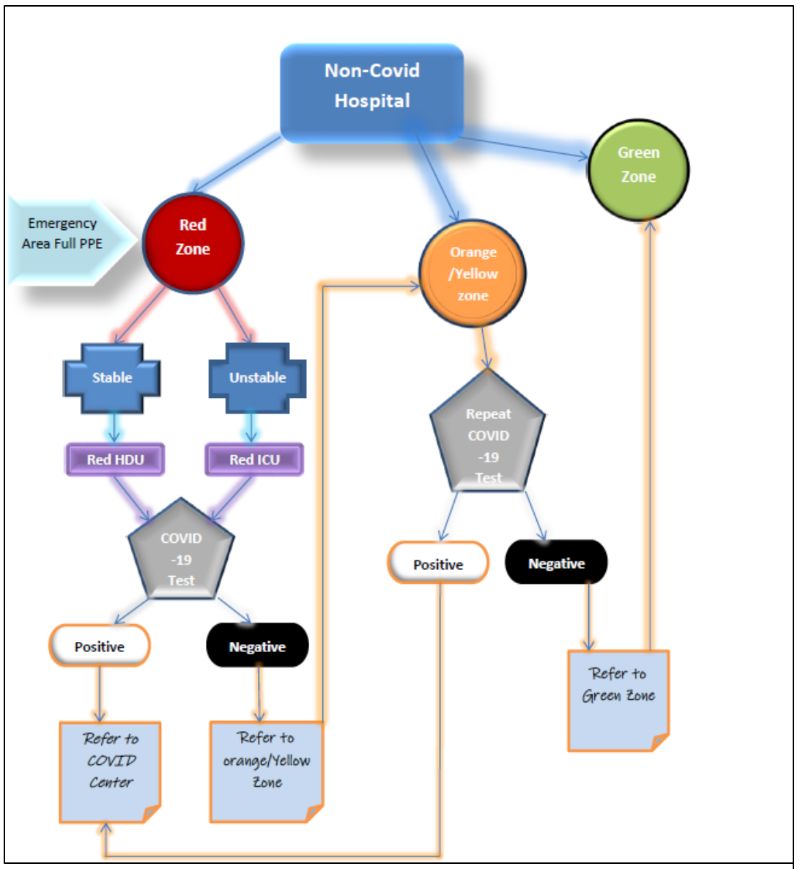
- Every center starts functioning in a ZONED MANNER i.e they get divided into zones viz. Red, Yellow and Green
- Functioning of Non-COVID Zoned Hospital (may have reserved bed for COVID-19)
INTRAHOSPITAL ZONING
Non-COVID ZONED HOSPITAL gets divided in the following:
- RED zone: Consists of Emergency Room , RED ICU and RED Ward
- Every HCW working in Red Zone works with all precautions including PPEs. (LEVEL 4)
- Patient treated as per his condition with all necessary monitoring and investigations thereby making things more clear
- First COVID-19 testing done at Red zone
- If patient is tested positive for COVID-19 then the patient is shifted to COVID center and if report comes out negative then patient is transferred to Yellow zone
- ORANGE or YELLOW zone: Consists of another ORANGE ICU and an ORANGE WARD
- Only patient once tested negative for COVID Negative gets entry to Yellow / Orange zone
- Health care workers use at least level 2 PPE adjunct with an antiviral kit
Patient are treated as per the symptoms with all necessary monitoring. - Clinical follow up of patient done with investigations like CBC to look for lymphopenia, coagulation profile to look for any derangement, LDH levels and serial Chest X-rays to look for radiological evidences .
- Also any suspected patient to be kept in isolation or cabin with Negative pressure if available
- Second COVID-19 testing done at Orange/ Yellow zone in case of any suspect either clinically or derangement in any of the significant investigations
- If patient is unfortunately tested Positive , patient is referred to COVID Unit
- If Second report also comes out Negative , then patient is transferred to Green zone
- GREEN zone: consists of GREEN ICU and GREEN Ward
- Patient that has been tested as COVID-19 negative twice is admitted in Green Zone
- HCWs use N95 and Gloves only
- Patients are treated as per his condition including all necessary monitoring and investigations
- Patients gets discharged from Green zone
ANTICIPATED CHALLENGES
- ZONING of the hospital itself may be a challenge as common AHUs . But this can be managed with little extra efforts and adequate planning and therefore allowing areas into a particular zone so that areas sharing common AHU comprise of either RED zone or Orange zone only
- Reallocation of healthcare workers in respective areas
- Rotational duty rosters and Post duty Quarantine followed by Covid testing before rejoining
- Additional cost of the PPE kits and additional Covid 19 test , this can sum up to around 8k- 10k per patient
- Adjunct Formulations
ANTICIPATED ADVANTAGES
- Protection of healthcare workers – with double testing and proper zoning of hospitals depending upon the risk associated, can achieve a system where minimize of the infection among HCWs by using proper PPEs depending upon the zones
- We will be able to cater to life-saving emergencies efficiently, also the routine services can be escalated with such kind of strategies
- The hospitals can achieve a system where they can provide their services near to normal (pre-covid times) thereby reaching a sustainable system both in terms of services and revenue generation
The current article mentions the zoning of a hospital for handling the emergency admissions, likewise for routine health services as well such zoning can be formulated and adopted. E.g. an elective surgery can be performed by performing a pre-admission COVID-19 test and then admitting the patient in ORANGE zone ward isolation rooms and then performing another test if required.
Recently there has been guidelines by Delhi govt suggesting a division of NonCovid hospitals into Risk Zones ( i.e mild , moderate, and severe ) addressing the issue of infection among HCWs and thereby suggesting the use of a different level of PPEs in different zones depending upon the risk associated . Also the advisory states formation of Holding area (corresponds to Red zone) for patients with influenza like illness (ILI ) in Non-Covid hospitals.
We appreciate the authorities for addressing the problem and taking such suggestions into consideration while forming the advisories and formulating the guidelines . Though there can be much more that can be done to achieve a more sustainable system which helps us fight the current pandemic in much more efficient manner as in our consideration achieving a SUSTAINABLE HEALTH SYSTEM ( HEALTH 2.0 ) is the only weapon amidst this crisis that can help us reach a safe bank.
Authored by Dr. Kulsaurabh & Dr. Yachika
Dr. Kulsaurabh is working as Intensivist at Fortis Escorts , New Delhi. Has done his MBBS and MD from PGIMS , Rohtak. Loves to be a part of an ecosystem working for any sought of development to overcome ongoing challenges. Presently holding a position as Joint Secretary, Federation of Resident Doctor association , FORDA.
Dr. Yachika completed MBBS from PGIMS Rohtak and has secured a respectable rank at NEET PG and will be joining a PG course.