
Dr Debbie Wake is a diabetologist, Clinical Reader at University of Edinburgh and Diabetes Consultant, (MBChB, BSc, PhD, Clin Ed Dip), and CEO and co-founder of MyWay Digital Health (MWDH). She leads national programmes on diabetes artificial intelligence/ international diabetes education programmes (Kuwait/ China). Previously, she was a health columnist for a national UK newspaper and TV doctor/ presenter for STVs ‘The Hour’ programme.
“new sensor-based technology that measures glucose (interstitially), through flash and continuous glucose monitoring (CGM) is transforming the lives of people with type 1 diabetes.”
Diabetes now affects around 9-10% of the global population/costing ~£500bn per year as per the study of International Diabetes Federation (IDF), with huge associated morbidity and mortality. As per the study of Grand View Research Reports, in parallel, the global digital health market is growing, and now totals over $206 billion, and by 2025 is expected to reach $509 billion. CAGR (compound annual growth rate) is 27.7%. Diabetes lends itself well to a digitally supported model of care delivery, and data-driven IT systems and digital applications may facilitate improved diabetes outcomes.
Internet-based technology can
- i) support people with diabetes directly, enabling better self-management (e.g. through internet linked apps supporting education, lifestyle or treatment titration)
- ii) support health care professionals to deliver better care through electronic health records, decision support, remote consultation tools, and population analytics.
In addition, new sensor-based technology that measures glucose (interstitially), through flash and continuous glucose monitoring (CGM) is transforming the lives of people with type 1 diabetes. Closed loop systems (i.e. continuous glucose monitors linked to insulin pumps, with dose adjustments driven by automated algorithms) are becoming the gold standard. Advanced glucose sensing technology is also showing promise for some aspects of type 2 diabetes management, although price currently inhibits widespread use.
The current COVID-19 epidemic (and poorer COVID outcomes in people with diabetes) has further increased the need for digital solutions, particularly technology which supports remote care models and population triage suggested in some scientific literature by Nagi and his team. Scalable remote technology based patient education approaches such as massive online open courses (MOOCs) may be highly cost effective (Mackenzie and team). Systematic literature reviews, evaluating use of digital tools and apps in diabetes self-management more generally, have demonstrated improvements in clinical outcomes, but show significant variability between interventions.
Data-Driven Care
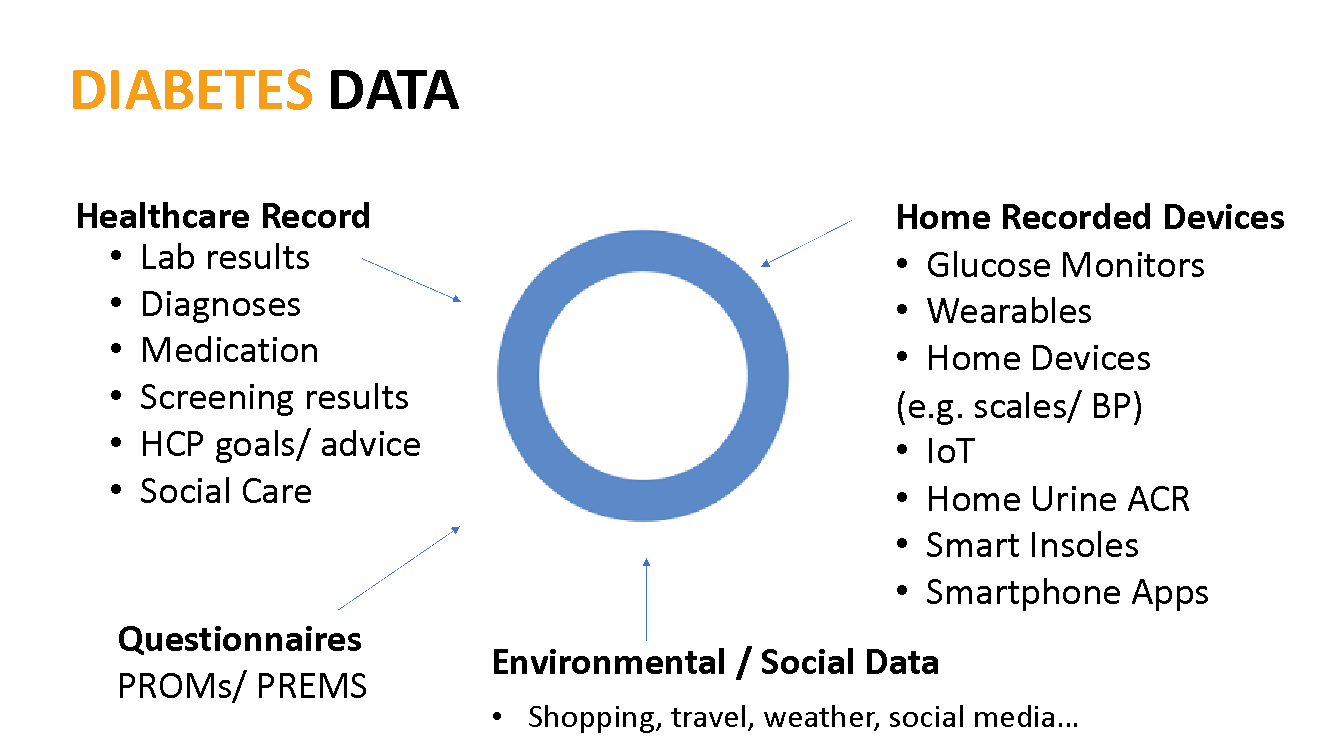
Gathering and exchanging data is key for any learning health system. Data in diabetes may come from electronic health records (e.g. demographics, clinic measurements, lab data, medication, appointments, past medical history etc.), screening programmes, and from patients directly through home devices such as activity monitors, glucose meters and increasingly through a plethora of home diagnostics and ‘internet of things’ sensors and devices. This may include foot pressure/ heat sensors to aid early detection of neuropathy, leading to foot ulcer prevention through to home urine testing linked to smartphone apps, to support detection of urine albumin. In addition, lifestyle and diet apps (including some with inbuilt food nutritional analysis are supporting day to day self-management decisions. Data may also come from questionnaires/ patient reported outcome/ experience measures (PROMs/PREMs),and other internet sources including social and environmental data.
The ability for a system to use data effectively to improve health care can be summarised by the informatics maturity model (table 1). The highest level (level 8) is associated with transformation of data and delivery to clinicians or patients through outputs which support a personalised precision medicine approach.
Precision Medicine /Decision Support
Using data to enable more personalised care, through data modelling and decision support could be transformative. A recent American Diabetes Association (ADA) /European Association for the Study of Diabetes (EASD) consensus report highlighted key areas where diabetes care is ready for precision diagnostics, therapeutics and prognostics, noting that “pragmatic studies of decision-support systems utilising rich information in health care systems… are needed”. Data-driven precision medicine in diabetes can support better diagnosis (including diabetes subtyping), more personalised prescribing (drug-response), and better prediction of short and long complications enabling early intervention. In addition, image-analysis AI is being used to support more rapid retinal image screening and for racking diabetic wound healing.
“To date, evidence for the use of Artificial Intelligence (AI)-driven decision support in clinical settings for chronic disease management remains limited. Data visualisation, or linked decision-support advice/ alerts can empower end users, i.e. turn data into knowledge and action. Clinical decision support (CDS) provides timely information, usually at the point of care, to help inform decisions about a patient’s care.”
To date, evidence for the use of Artificial Intelligence (AI)-driven decision support in clinical settings for chronic disease management remains limited. Data visualisation, or linked decision-support advice/ alerts can empower end users, i.e. turn data into knowledge and action. Clinical decision support (CDS) provides timely information, usually at the point of care, to help inform decisions about a patient’s care. A recent meta-analysis (BMJ) demonstrated that clinical decision support interventions in a more general setting achieve small to moderate improvements in targeted processes of care, with limited evidence to date demonstrating improved clinical outcomes. The paper calls for a human factors approach to understand workflows, patient-orientated support, and the use of AI to improve prediction, and preventative care decision support.
“Data is made available for clinical use, audit, research and patient self-management. The use of a national data platform in Scotland has been associated with significant improvements in care quality and outcomes.”
Case Study (Scotland)
Over the past 20 years, Scotland has taken a national approach to diabetes management underpinned by exchanging linked data. The national SCI-Diabetes platform which is accessible to all clinicians in Scotland who manage diabetes, exchanges data from all primary care clinics, national laboratory data and national screening programmes. Data exchange is possible through the use of a unique patient identifier [Community Health Index (CHI)]. Data is made available for clinical use, audit, research and patient self-management. The use of a national data platform in Scotland has been associated with significant improvements in care quality and outcomes.
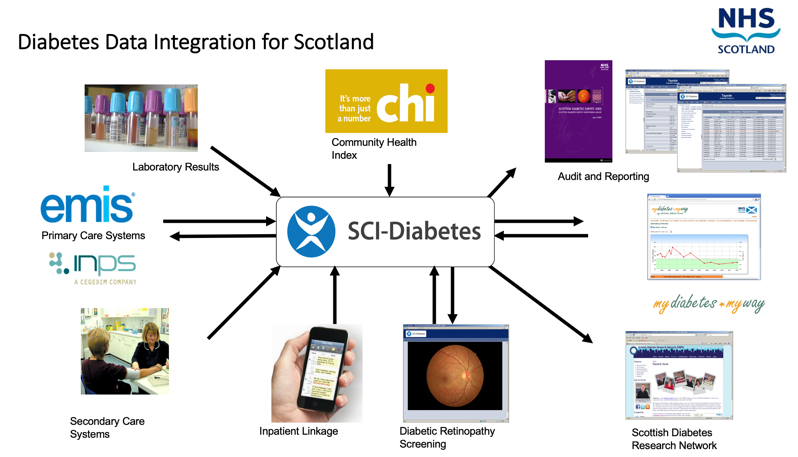
Legend: Schemata of national diabetes data integration in Scotland coordinated through the central (SCI-diabetes) clinical IT platform.
Rules-based decision support tools embedded in SCI-diabetes (the national clinical diabetes platform; https://www.sci-diabetes.scot.nhs.uk)) further delivered a 3-4x improved compliance with national medical guidelines.
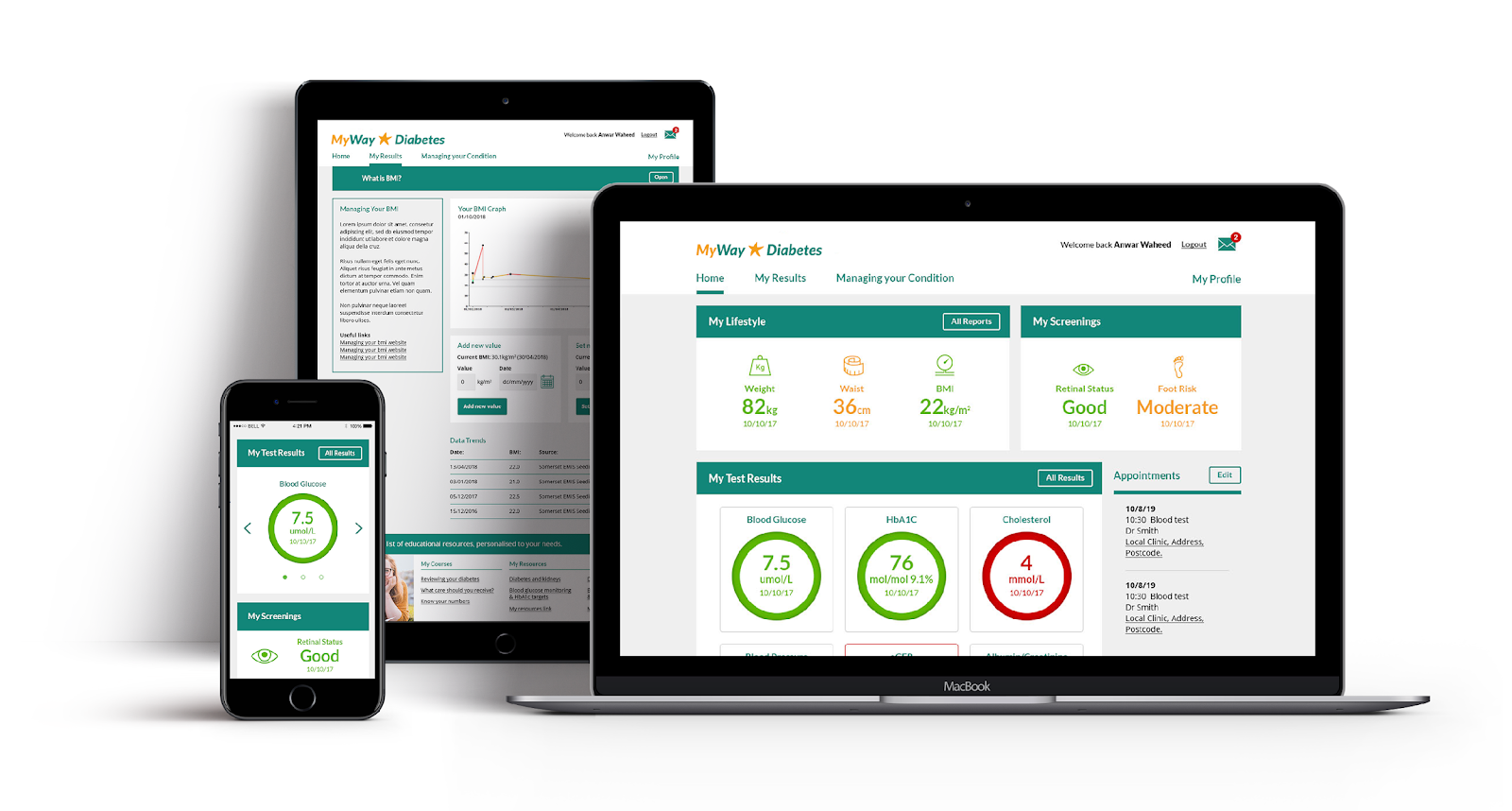
My Diabetes My Way (now MyWay Diabetes)
SCI-diabetes data is made available to patients through Scotland’s MyDiabetesMyWay (MDMW) patient data access and education platform. Around 500,000 people have used the MDMW website and >60,000 registered for data access (since 2010). This platform also supports online structured education courses. MDMW use has been associated with improvements in key parameters such as HbA1c and cost-savings with ~ 5:1 return on investment. More advanced AI-driven predictive analytics and linked decision support is currently being tested; supported by MyWay Digital Health.
“Population management systems can further focus care toward those in most need. Data-driven solutions have the potential to reduce mortality, morbidity, reduce complications, drive more effective treatment prescriptions, improve quality of life, improve patient safety, enable more effective diagnosis and prescribing and delivery system efficiencies.”
Summary
Digital technologies and data could have wide benefits for people with diabetes and other long-term conditions, enabling better personalised self-management, scaled through internet-based delivery. In addition, given the high prevalence of diabetes, most care is provided by generalists, who may lack specialist knowledge; accessible guideline-linked evidence-based decision support, could be a great enabler. Population management systems can further focus care toward those in most need. Data-driven solutions have the potential to reduce mortality, morbidity, reduce complications, drive more effective treatment prescriptions, improve quality of life, improve patient safety, enable more effective diagnosis and prescribing and delivery system efficiencies. Investment in underlying infrastructure and policies to support data standardisation, interoperability, information governance is essential to realise these benefits, and ongoing research is encouraged to better understand the impact.

